Blood sugar
The blood sugar concentration or blood glucose level is the amount of glucose (sugar) present in the blood of a human or animal. Normally in mammals, the body maintains the blood glucose level at a reference range between about 3.6 and 5.8 mM (mmol/L, i.e., millimoles/liter) (64.8 and 104.4 mg/dL). Blood glucose levels are tightly regulated as a part of metabolic homeostasis.
Glucose is the primary source of energy for the body's cells, and blood lipids (in the form of fats and oils) are primarily a compact energy store. Glucose is transported from the intestines or liver to body cells via the bloodstream, and is made available for cell absorption via the hormone insulin, produced by the body primarily in the pancreas.
The mean normal blood glucose level in humans is about 4 mM (4 mmol/L or 72 mg/dL, i.e. milligrams/deciliter); however, this level fluctuates throughout the day. Glucose levels are usually lowest in the morning, before the first meal of the day (termed "the fasting level"), and rise after meals for an hour or two by a few grams.
Blood sugar levels outside the normal range may be an indicator of a medical condition. A persistently high level is referred to as hyperglycemia; low levels are referred to as hypoglycemia. Diabetes mellitus is characterized by persistent hyperglycemia from any of several causes, and is the most prominent disease related to failure of blood sugar regulation. A temporarily elevated blood sugar level may also result from severe stress, such as trauma, stroke, myocardial infarction, surgery, or illness. Intake of alcohol causes an initial surge in blood sugar, and later tends to cause levels to fall. Also, certain drugs can increase or decrease glucose levels.[1]
Contents |
Blood glucose measurement units
The international standard way of measuring blood glucose levels are in terms of a molar concentration, measured in mmol/L (millimoles per litre; or millimolar, abbreviated mM). In the United States, mass concentration is measured in mg/dL (milligrams per decilitre).[2]
Since the molecular weight of glucose C6H12O6 is about 180 g/mol, for the measurement of glucose, the difference between the two scales is a factor of 18, so that 1 mmol/L of glucose is equivalent to 18 mg/dL.[3]
Normal values
Many factors affect a person's blood sugar level. A body's homeostatic mechanism, when operating normally, restores the blood sugar level to a narrow range of about 82 to 110 mg/dL (4.4 to 6.1 mmol/L).
Despite widely variable intervals between meals or the occasional consumption of meals with a substantial carbohydrate load, human blood glucose levels normally remain within the normal range. However, shortly after eating the blood glucose level may rise temporarily up to 140 mg/dL (7.8 mmol/L) or a bit more in non-diabetics. The American Diabetes Association recommends a post-meal glucose level less than 180 mg/dl (10 mmol/L) and a pre-meal plasma glucose of 90–130 mg/dL (5 to 7.2 mmol/L).[4]
The actual amount of glucose in the blood and body fluids is very small. The control mechanism in the human body works on very small quantities of glucose. In a healthy adult male of 165 lb (75 kg) with a blood volume of 1.3 gal (5 litres), a blood glucose level of 100 mg/dL or 5.5 mmol/L corresponds to about 5 g (0.2 oz or 0.002 gal, 1/500 of the total) of glucose in the blood and approximately 45 g (1½ ounces) in the total body water (which includes more than merely blood and will be usually about 60% of the total body weight in men). (Small sugar packets provided in many restaurants with coffee or tea are about 2.8 grams each.[5])
Regulation
The body's homeostatic mechanism keeps blood glucose levels within a narrow range. It is composed of several interacting systems, of which hormone regulation is the most important.
There are two types of mutually antagonistic metabolic hormones affecting blood glucose levels:
- catabolic hormones (such as glucagon, growth hormone, cortisol and catecholamines) which increase blood glucose;
- and one anabolic hormone (insulin), which decreases blood glucose.
Health effects
If blood sugar levels drop too low, a potentially fatal condition called hypoglycemia develops. Symptoms may include lethargy, impaired mental functioning, irritability, shaking, twitching, weakness in arm and leg muscles, pale complexion, sweating, paranoid or aggressive mentality and loss of consciousness. Brain damage is even possible.
If levels remain too high, appetite is suppressed over the short term. Long-term hyperglycemia causes many of the long-term health problems associated with diabetes, including eye, kidney, heart disease and nerve damage.
Low blood sugar
Mechanisms that restore satisfactory blood glucose levels after hypoglycemia must be quick and effective to prevent extremely serious consequences of insufficient glucose: confusion or unsteadiness, and, in the extreme, coma. It is far more dangerous to have too little glucose in the blood than too much, at least temporarily. In healthy individuals, blood glucose-regulating mechanisms are generally quite effective, and symptomatic hypoglycemia is generally only found in diabetics using insulin or other pharmacological treatment. Hypoglycemic episodes can vary greatly between persons and from time to time, both in severity and swiftness of onset. For severe cases, prompt medical assistance is essential, as damage to brain and other tissues and even death will result from sufficiently low blood glucose levels.
Some healthy individuals report drowsiness or impaired cognitive function several hours after meals, which they believe is related to a drop in blood sugar, or low blood sugar. For more information, see:
- idiopathic postprandial syndrome
- hypoglycemia
Comparative content

Glucose measurement
Sample type
Glucose is measured in whole blood or serum . Historically, blood glucose values were given in terms of whole blood, but most laboratories now measure and report the serum glucose levels. Because red blood cells (erythrocytes) have a higher concentration of protein (e.g., hemoglobin) than serum, serum has a higher water content and consequently more dissolved glucose than does whole blood. To convert from whole-blood glucose, multiplication by 1.15 has been shown to generally give the serum/plasma level.
Collection of blood in clot tubes for serum chemistry analysis permits the metabolism of glucose in the sample by blood cells until separated by centrifugation. Red blood cells, for instance, do not require insulin to intake glucose from the blood. Higher than normal amounts of white or red blood cell counts can lead to excessive glycolysis in the sample with substantial reduction of glucose level if the sample is not processed quickly. Ambient temperature at which the blood sample is kept prior to centrifuging and separation of plasma/serum also affects glucose levels. At refrigerator temperatures, glucose remains relatively stable for several hours in a blood sample. At room temperature (25 °C), a loss of 7-10 mg/dL (or 0.4 mmol/L) of total glucose per hour should be expected in whole blood samples. Loss of glucose under these conditions can be prevented by using Fluoride tubes (i.e., gray-top) since fluoride inhibits glycolysis. However, these should only be used when blood will be transported from one hospital laboratory to another for glucose measurement. Red-top serum separator tubes also preserve glucose in samples after being centrifuged isolating the serum from cells.
Particular care should be given to drawing blood samples from the arm opposite the one in which an intravenous line is inserted, to prevent contamination of the sample with intravenous fluids. Alternatively, blood can be drawn from the same arm with an IV line after the IV has been turned off for at least 5 minutes, and the arm elevated to drain infused fluids away from the vein. Inattention can lead to large errors, since as little as 10% contamination with 5% dextrose (D5W) will elevate glucose in a sample by 500 mg/dl or more. Remember that the actual concentration of glucose in blood is very low, even in the hyperglycemic.
Arterial, capillary and venous blood have comparable glucose levels in a fasting individual. After meals venous levels are somewhat lower than capillary or arterial blood; a common estimate is about 10%.
Measurement techniques
Two major methods have been used to measure glucose. The first, still in use in some places, is a chemical method exploiting the nonspecific reducing property of glucose in a reaction with an indicator substance that changes color when reduced. Since other blood compounds also have reducing properties (e.g., urea, which can be abnormally high in uremic patients), this technique can produce erroneous readings in some situations (5 to 15 mg/dl has been reported). The more recent technique, using enzymes specific to glucose, are less susceptible to this kind of error. The two most common employed enzymes are glucose oxidase and hexokinase.
In either case, the chemical system is commonly contained on a test strip, which is inserted into a meter, and then has a blood sample applied. Test strip shapes and their exact chemical composition vary between meter systems and cannot be interchanged. Formerly, some test strips were read (after timing and wiping away the blood sample) by visual comparison against a color chart printed on the vial label. Strips of this type are still used for urine glucose readings, but for blood glucose levels they are obsolete. Their error rates were, in any case, much higher.
Urine glucose readings, however taken, are much less useful. In properly functioning kidneys, glucose does not appear in urine until the renal threshold for glucose has been exceeded. This is substantially above any normal glucose level, and so is evidence of an existing severe hyperglycemic condition. However, urine is stored in the bladder and so any glucose in it might have been produced at any time since the last time the bladder was emptied. Since metabolic conditions change rapidly, as a result of any of several factors, this is delayed news and gives no warning of a developing condition. Blood glucose monitoring is far preferable, both clinically and for home monitoring by patients.
| I. CHEMICAL METHODS | ||
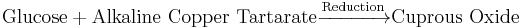
| A. Oxidation-Reduction Reaction | ||
 |
||
| 1. Alkaline Copper Reduction | ||
| Folin Wu Method | 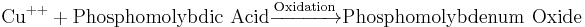 |
Blue end-product |
| Benedict's method |
|
|
| Nelson Somogyi Method | 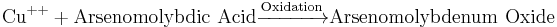 |
Blue end-product |
| Neocuproine Method | 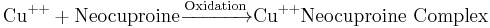 * * |
Yellow-orange color Neocuproine |
| Shaeffer Hartmann Somogyi |
|
|
| 2. Alkaline Ferricyanide Reduction | ||
| Hagedorn Jensen | 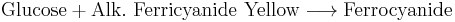 |
Colorless end product; other reducing substances interfere with reaction |
| B. Condensation | ||
| Ortho-toluidine Method |
|
|
| Anthrone (Phenols) Method |
|
|
| II. ENZYMATIC METHODS | ||
| A. Glucose Oxidase | ||
![\mathrm{Glucose} + \mathrm{O}^{2}\xrightarrow[\mathrm{Oxidation}] {\mathrm{glucose\ oxidase}}\mathrm{Cuprous\ Oxide}](/2010-wikipedia_en_wp1-0.8_orig_2010-12/I/ee4b420e1c8f2445a89e73f63727897d.png) |
||
| Saifer–Gerstenfeld Method | ![\mathrm{H_{2}O_2} + \textrm{\textit{O}-dianisidine}\xrightarrow[\mathrm{Oxidation}] {\mathrm{peroxidase}} \mathrm{H_2O} + \mathrm{oxidized\ chromogen}](/2010-wikipedia_en_wp1-0.8_orig_2010-12/I/e563e5405afc63ea175af0bdcdce58e3.png) |
Inhibited by reducing substances like BUA, Bilirubin, Glutathione, Ascorbic Acid |
| Trinder Method |
|
|
| Kodak Ektachem |
|
|
| Glucometer |
|
|
| B. Hexokinase | ||
|
|
||
|
||
Blood glucose laboratory tests
- fasting blood sugar (i.e., glucose) test (FBS)
- urine glucose test
- two-hr postprandial blood sugar test (2-h PPBS)
- oral glucose tolerance test (OGTT)
- intravenous glucose tolerance test (IVGTT)
- glycosylated hemoglobin (HbA1C)
- self-monitoring of glucose level via patient testing
Clinical correlation
The fasting blood glucose level, which is measured after a fast of 8 hours, is the most commonly used indication of overall glucose homeostasis, largely because disturbing events such as food intake are avoided. Conditions affecting glucose levels are shown in the table below. Abnormalities in these test results are due to problems in the multiple control mechanism of glucose regulation.
The metabolic response to a carbohydrate challenge is conveniently assessed by a postprandial glucose level drawn 2 hours after a meal or a glucose load. In addition, the glucose tolerance test, consisting of several timed measurements after a standardized amount of oral glucose intake, is used to aid in the diagnosis of diabetes. It is regarded as the gold standard of clinical tests of the insulin / glucose control system, but is difficult to administer, requiring much time and repeated blood tests. In comparison, the fasting blood glucose level is a much poorer screening test because of the high variability of the experimental conditions such as the carbohydrate content of the last meal and the energy expenditure between the last meal and the measurement. Actually, many people with prediabetes or diabetes can have a fasting blood glucose below the prediabetic/diabetic threshold if their last meal happened to be low in carbohydrate and they burnt all the related glucose in their blood stream before taking the test. Note that food commonly includes carbohydrates which don't participate in the metabolic control system; simple sugars such as fructose, many of the disaccarhides (which either contain simple sugars other than glucose or cannot be digested by humans) and the more complex sugars which also cannot be digested by humans. And there are carbohydrates which are not digested even with the assistance of gut bacteria; several of the fibres (soluble or insoluble) are chemically carbohydrates. Food also commonly contains components which affect glucose (and other sugar's) digestion; fat, for example slows down digestive processing, even for such easily handled food constituents as starch. Avoiding the effects of food on blood glucose measurement is important for reliable results since those effects are so variable.
Error rates for blood glucose measurements systems vary, depending on laboratories, and on the methods used. Colorimetry techniques can be biased by color changes in test strips (from airborne or finger borne contamination, perhaps) or interference (e.g., tinting contaminants) with light source or the light sensor. Electrical techniques are less susceptible to these errors, though not to others. In home use, the most important issue is not accuracy, but trend. Thus if your meter / test strip system is consistently wrong by 10%, there will be little consequence, as long as changes (e.g., due to exercise or medication adjustments) are properly tracked. In the US, home use blood test meters must be approved by the Federal Food and Drug Administration before they can be sold.
Finally, there are several influences on blood glucose level aside from food intake. Infection, for instance, tends to change blood glucose levels, as does stress either physical or psychological. Exercise, especially if prolonged or long after the most recent meal, will have an effect as well. In the normal person, maintenance of blood glucose at near constant levels will nevertheless be quite effective.
| Persistent Hyperglycemia | Transient Hyperglycemia | Persistent Hypoglycemia | Transient Hypoglycemia |
|---|---|---|---|
| Reference Range, FBG: 70–110 mg/dl | |||
| Diabetes Mellitus | Pheochromocytoma | Insulinoma | Acute Alcohol Ingestion |
| Adrenal cortical hyperactivity Cushing's Syndrome | Severe Liver Disease | Adrenal cortical insufficiency Addison's Disease | Drugs: salicylates, antituberculosis agents |
| Hyperthyroidism | Acute stress reaction | Hypopituitarism | Severe Liver disease |
| Acromegaly | Shock | Galactosemia | Several Glycogen storage diseases |
| Obesity | Convulsions | Ectopic Insulin production from tumors | Hereditary fructose intolerance |
Etymology and use of term
The term 'blood sugar' has colloquial origins. In a physiological context, the term is a misnomer because it refers to glucose, yet other sugars besides glucose are always present. Food contains several different types (e.g., fructose (largely from fruits/table sugar/industrial sweeteners). galactose (milk and dairy products), as well as several food additives such as sorbitol, xylose, maltose, ...). But because these other sugars are largely inert with regard to the metabolic control system (i.e., that controlled by insulin secretion), since glucose is the dominant controlling signal for metabolic regulation, the term has gained currency, and is used by medical staff and lay folk alike. The table above reflects some of the more technical and closely defined terms used in the medical field.
Blood glucose in birds and reptiles
In birds and reptiles the processing of sugars is done differently, the pancreas is slightly more well developed in birds than in mammals, perhaps as a partial compensation for the lack of saliva and chewing. It produces carbohydrate, fat and protein digesting enzymes which are secreted into the small intestine. The liver has two distinct lobes each with its own duct leading into the small intestine. The liver, as in mammals, houses the bile, which in birds however is acidic and not alkaline as it is in mammals. Many birds do not have a gall bladder to hold the bile, and it is secreted directly into the pancreatic ducts.
References
- ↑ Type 2 Diabetes - Your Questions Answered, by Rosemary Walker & Jill Rodgers, ISBN 1-74033-550-3.
- ↑ Diabetes FAQs - Blood Glucose Measurement Units - Abbott Diabetes Care
- ↑ What are mg/dl and mmol/l? How to convert? Glucose? Cholesterol?
- ↑ American Diabetes Association. January 2006 Diabetes Care. "Standards of Medical Care-Table 6 and Table 7, Correlation between A1C level and Mean Plasma Glucose Levels on Multiple Testing over 2-3 months." Vol. 29 Supplement 1 Pages 51-580.
- ↑ USDA National Nutrient Database for Standard Reference, Release 22 (2009)
Further reading
- John Bernard Henry, M.D.: Clinical diagnosis and Management by Laboratory Methods 20th edition, Saunders, Philadelphia, PA, 2001.
See also
- Current research - Boronic acids in supramolecular chemistry: Saccharide recognition
- Blood glucose monitoring
- Glucagon
|
||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||

![\begin{alignat}{2}
& \mathrm{Glucose} + \mathrm{ATP}\xrightarrow[\mathrm{Phosphorylation}] {\mathrm{Hexokinase} + \mathrm{Mg}^{++}} \textrm{G-6PO}_4 + \mathrm{ADP} \\
& \textrm{G-6PO}_4 + \mathrm{NADP}\xrightarrow[\mathrm{Oxidation}] {\textrm{G-6PD}} \textrm{G-Phosphogluconate} + \mathrm{NADPH} + \mathrm{H}^{+} \\
\end{alignat}](/2010-wikipedia_en_wp1-0.8_orig_2010-12/I/55e5b2ebdbaddaf4c69d398449ddf479.png)